Author: Dr. Alessio liberati
Impaired movement and walking due to a chronic and evolutionary course: this is what lies behind Parkinson's disease. People affected by this pathology often have difficulty walking and maintaining balance, and the progression of symptoms exposes them more to the fall risk. In fact, it is estimated that about 60-80% of people affected by this disease fall at least once a year.
The causes can be multiple:
- less efficient postural reflexes
- increased reaction time
- reduced blood pressure
- altered posture
Only a suitable therapeutic path – supported by an objective evaluation – can improve the patient's autonomy and quality of life, trying to stem the problem.
Technology, as always, comes to our aid. Thanks to motion sensors such as baiobit, it is possible to carry out precise and fast measurements to identify multiple parameters, some of which cannot be detected through observation, for example:
- the displacements of the Center of Mass (COM) during the monopodalic balance tests;
- the duration of the individual phases of the Timed Up and Go test;
- the space-time parameters of the walk (eg. swing phase, stance phase, etc.).
All useful elements for the physiotherapist to plan a patient-oriented rehabilitation process.
Anamnesis
71-year-old man suffering from Parkinson's disease, with important conditioning in the activities of daily living.
The patient presents:
- muscle stiffness and camptocormic attitude that leads to the phenomenon of gait festination;
- increase in festination with increasing distance during walking;
- evident tremor in the upper limbs during the tests, especially in the right upper limb.
Assessment
The physical-clinical examination revealed both a marked stiffness of the postural muscles and the presence of the "trochlea dentata" phenomenon in passive movements, especially in the upper limbs: both alarm bells of possible accidental falls.
The fall risk can be determined by several factors:
- Age over 65 years
- Previous falls
- Visual impairment
- Medicines
- Cognitive impairment
- Motor
In this context, the motor risk factors, related to walking and balance, represent important indices to be considered in order to predict future falls. The baiobit system works precisely in this direction, returning data relating to motor difficulties relating to strength, balance and stability during walking (see table 1), thanks to three simple and quick tests:
- Timed Up and Go
- Walking
- Balance
| Test | Description | Indexes | Alert values | Notes |
| Timed Up and Go | Fall risk and motor abilities evaluation in the different phases: sitting-to-standing, sitting, walking and turning | Total time necessary for the test execution | In the event of Parkinson's disease < 11,5 s | In the event of a high fall risk, it is essential to examine the
individual phases and set up a rehabilitation program aimed at
recovering the deficits highlighted.
Sit-to-stand phase: identifies a possible lack of strength in the lower limbs:
Walking phase (round trip): identifies a cautious gait with a reduced speed. It is useful to deepen the walk test.
Breakthrough phase (firs and second): identifies a possible balance difficulty.
Session phase: identifies a possible lack of strength in the lower limbs and poor control of the eccentric phase. |
| Walking test | Gait evaluation, aimed at measuring its stability | Speed | < 1 m/s | Speeds below one meter per second are indicative of an increased fall
risk, therefore it is important to set up a rehabilitation program aimed
at improving stability |
| | Walking Ratio (WR) | < 66,5 mm*min/step | If lower than 6.5 it indicates a cautious pace. Also to be evaluated in
relation to stride length, cadence and duration of the stance phase.
Reduced stride length values, normalized to the height of the subject,
could be indicative of a search for stability |
| Balance test (rh/lh) | Monopodalic Load Stability balance test, for the evaluation of stability in static conditions | Fall index according to Springer, in relation to te time in which the subject is able to mantain the monopodalic load | In the event of a subject aged T < 28,7 s | Highlights a problem of balance in single-stance load, and in the
management of balance that could affect walking skills and the
performance of activities of daily life (ADL) |
| | Ellipse area | Test global performance | Comparison of the left and right lower limbs can highlight important asymmetries in the management of balance |
Table 1The patient in need of a fall risk assessment is subjected to several tests: the higher the number of tests that fail, the higher the chances for him to fall. Even if only one test fails, the patient is to be considered exposed to the fall risk and therefore must follow an exercise path suitable for recovering full stability.
Rehabilitation program
In this case, the results of the tests performed (see table 2) showed a high fall risk:
| Test | Result | baiobit test result | Notes |
| Timed Up and Go test (Fig.1) | Failed | Total time = 12,63 s | Greater difficulties during the walking phase where a longer than normal time is evident |
| Left monopodalic fall risk test (Fig. 2) | Failed | Time = 12 s
Ellipse area = 908 mm2 | There is instability of the static balance in bilateral monopodalic load, with a greater deficit on the left |
| Right monopodalic fall risk test (Fig. 3) | Failed | Time = 7 s
Ellipse area = 515 mm2 | There is instability of the static balance in bilateral monopodalic load, with a greater deficit on the left |
| Walking test (fig.4)
| Failed | Speed = 0,7 m/s
WR = 71,71 mm*min/step | There is difficulty in walking with a significant decrease in cadence
and step length, associated with a decrease in the duration of the
bilateral swing phase, probably due to the difficulty of managing the
single-stance load |
Table 2Considering balance difficulties in the static and dynamic phase, the following rehabilitation program has been established, lasting about three months:
- neurocognitive exercises (ETC);
- fascial manipulation to decrease muscle stiffness;
- neuromuscular taping with the aim of improving the perception and management of muscle stiffness;
- therapeutic exercises with baiobit supported by biofeedback:
– exercises of dynamic balance to favor a better management of the center of mass during the movements of the body (such as getting up / sitting down from the chair and during changes of direction);
– Joint Position Sense exercises on the rotation of the trunk during the walk, in order to favor a correct release of the tracks during the gait cycles;
– Cervical Clock for improving the perception of cervical movements.
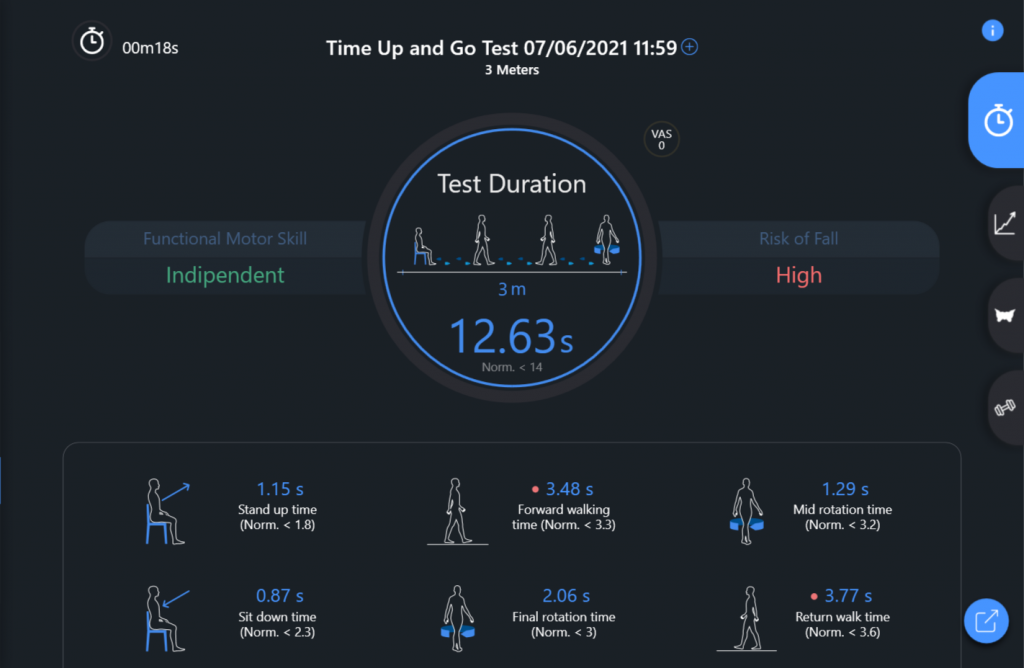 Fig. 1
Fig. 1
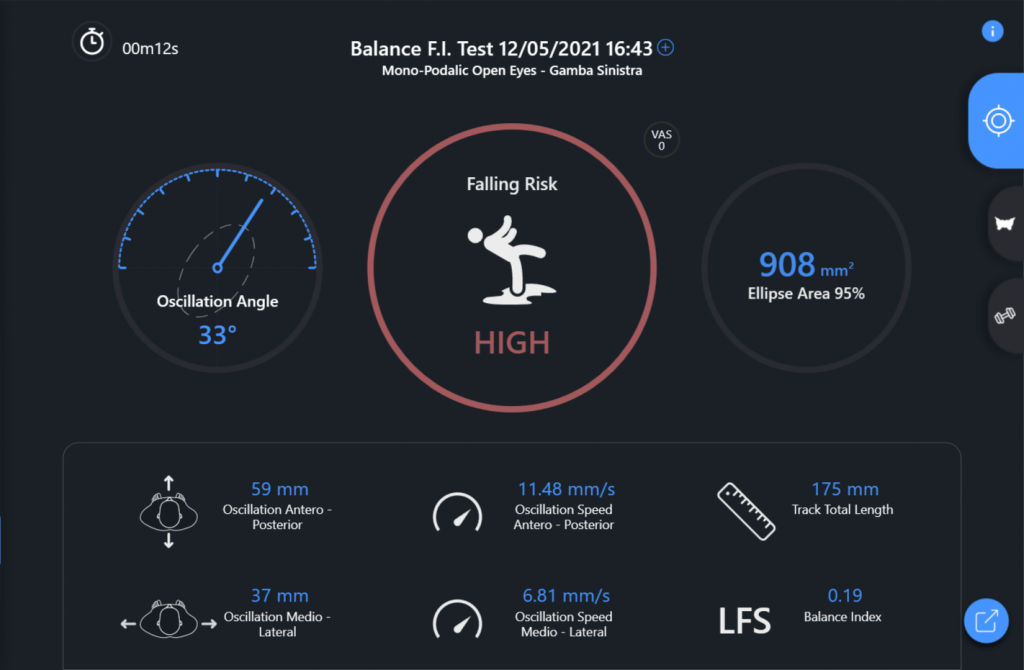 Fig. 2
Fig. 2
 Fig. 3
Fig. 3
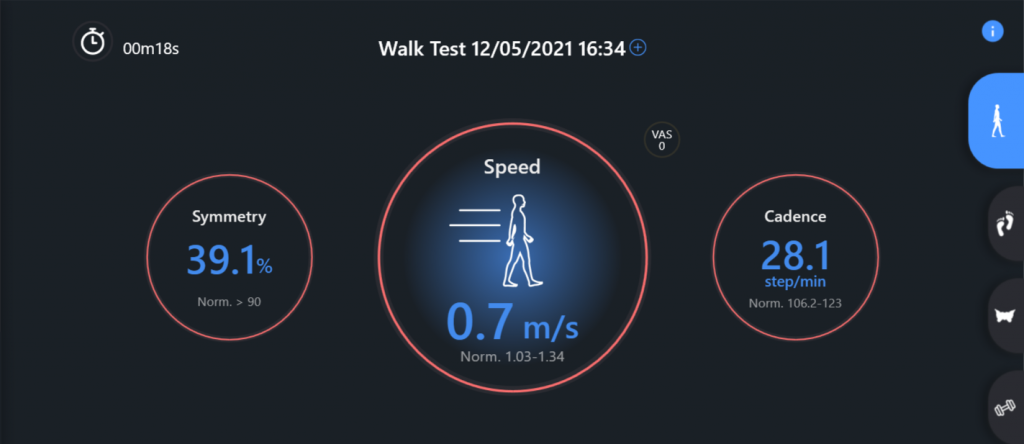 Fig. 4
Fig. 4
Results
At the end of the rehabilitation, the evaluation tests with baiobit were repeated to quantify the progress obtained by the patient (see table 3), comparing these reports with the initial ones.
| Test | Result | baiobit test result | Notes |
| Timed Up and Go test (Fig.5) | Successful | Total time = 10,98 s | Generalized improvement in all phases of the test, in fact all phases are now included in the reference values provided |
| Left monopodalic fall risk test (Fig. 6) | Failed | Time = 16 s
Ellipse area = 2382 mm2 | High fall risk due to both the lower right and lower left limbs, it will
therefore be necessary to continue the work in order to improve the
static balance |
| Right monopodalic fall risk test (Fig. 7) | Failed | Time = 5 s
Ellipse area = 760 mm2 | High fall risk due to both the lower right and lower left limbs, it will
therefore be necessary to continue the work in order to improve the
static balance |
| Waling test (fig.8) | Failed | Speed = 0,58 m/s
WR = 5,19 mm*min/step | It is necessary to continue the rehabilitation process to seek a further improvement of the gait pattern |
Table 3 Fig. 5
Fig. 5
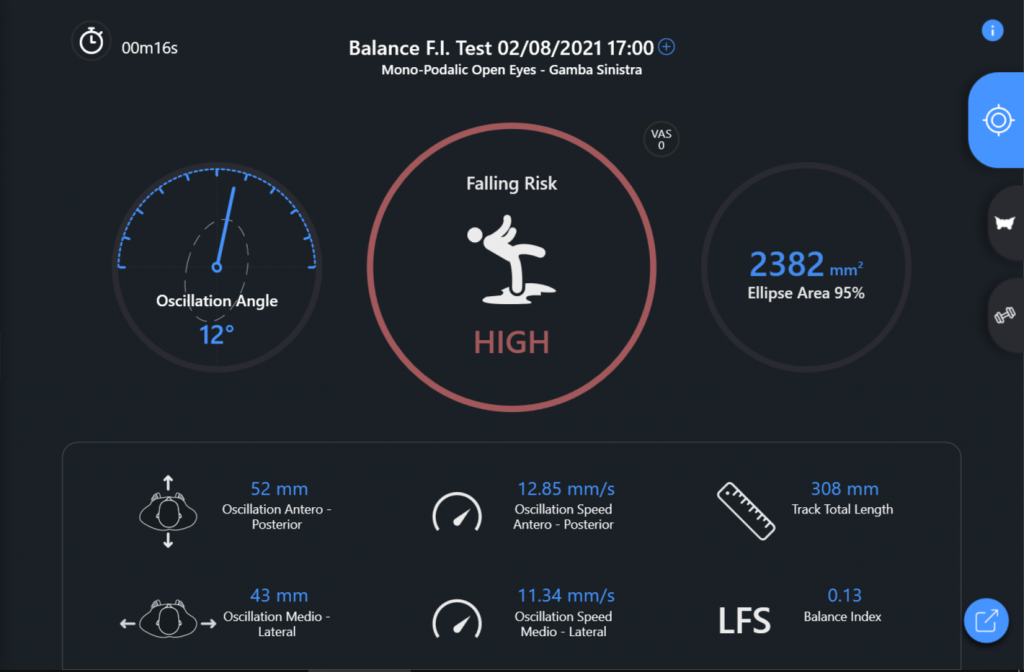 Fig. 6
Fig. 6
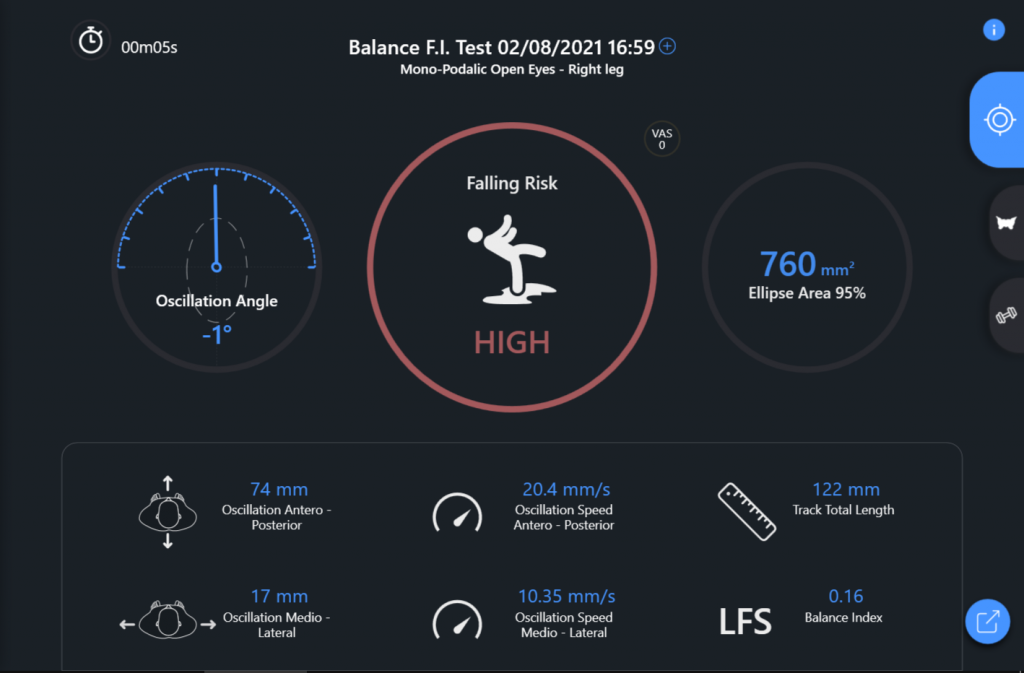 Fig. 7
Fig. 7
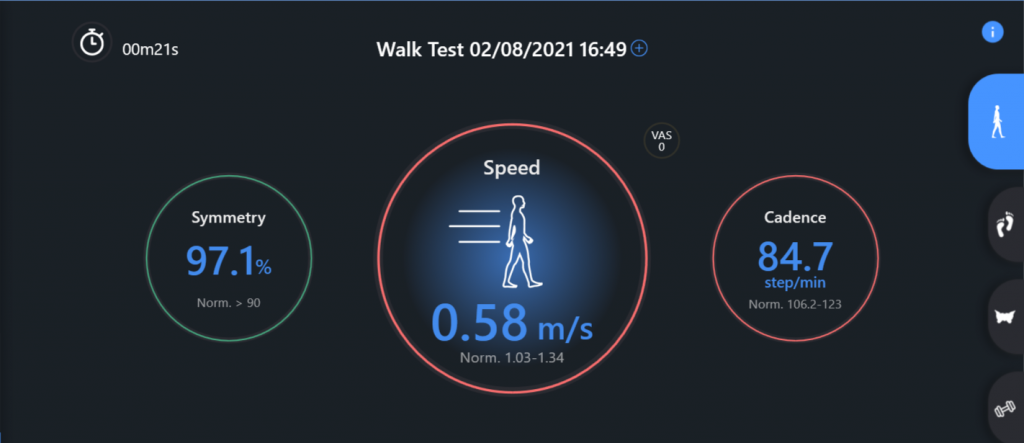 Fig. 8
Fig. 8
In particular, the comparison of the Timed Up and Go test, pre and post rehabilitation path, shows an improvement in the management of ADL (getting up, sitting down …)
On the other hand, an unfavorable condition remains in the balance and walking tests, which highlights the need to continue the program focusing on the management of the single-stance load.
Conclusion
Thanks to the use of baiobit technology, capable of accurately identifying the difficulties of the Parkinsonian patient, it was possible to objectively assess the fall risk and implement a patient-oriented rehabilitation program supported by biofeedback exercises.