According to the data from the Italian Society of Orthopedics and Traumatology (Siot), more than 85,000 knee prostheses are implanted every year.
However, if we consider not only the single prosthetic interventions but also the several interventions placed for prosthesis fixation, this value will be higher.
Over the years, the less invasive surgical techniques and the technological evolution of the tools used have allowed considerable progress (1). Despite this, adequate rehabilitation therapy remains essential to allow maximum functional recovery (2).
The objectives that the rehabilitation process must accomplish are as follows (2):
- manage post-operative pain;
- restore the knee ROM, allowing the achievement of 110 degrees of flexion, a measure that constitutes a satisfactory function to carry out most of the activities of daily life (4);
- restore the muscular strength of the lower limb;
- restore the ability to walk in total comfort and without symptoms;
- develop functional independence;
- restore the ability to participate in activities of daily living.
A common consensus emerges towards an early rehabilitation path that focuses on performing active physical exercises (5), allowing the above objectives to be achieved in the shortest time.
Among the recommended active exercise techniques, active aquatic therapy is recommended for the return of function and motor gestures (6).
ANANMNESIS
56-year-old man undergoing surgery for patellar fracture and external tibial plateau, implantation of plates and screws to the tibia and cerclage to the patella. The trauma occurred on June 10, 2021 and the subject underwent surgery on June 25, 2021.
ASSESSMENT
The patient is brought to our attention on October 5, 2021, at the first physical examination showing:
- scar adhesions
- hypomobile patella
- diffuse hypotrophy to the operated limb
- distal edema
- difficulty in walking with the help of 1 Canadian cane.
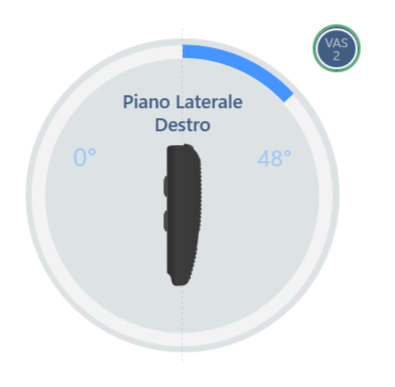
An evaluation of the knee joint ROM is also performed with the support of baiobit, by which it was detected (Figure 1):
• passive flexion equal to 48° with slight pain VAS 2/10.
REHABILITATION PROGRAM
It is recommended to start a cycle of hydrokinesitherapy with a frequency of 3 times a week with 2 main objectives:
- ROM improvement
- restoration of a correct outline of the gait cycle.
Given the considerable limitation of the knee joint mobility, especially in flexion, the first part of the rehabilitation program focuses on restoring this aspect. In each session, muscle stretching and joint release exercises are alternated with proprioceptive exercises and gait cycle rehabilitation.
At the end of this first phase, a re-evaluation of the joint ROM was carried out to monitor the actual improvement obtained.
In addition, a gait analysis was carried out with baiobit which made it possible to highlight the alterations of the gait cycle and create a targeted rehabilitation program that allows the design of exercises suitable for restoring correct walking without aids and without compensation.
RESULTS
At the end of the first phase, the knee joint mobility was then reassessed through a new baiobit test which shows that now the knee flexion is 83°, thus highlighting an improvement in flexion joint mobility of 78% (Figure 2).

Finally, the Walk Test with baiobit was performed to plan the second part of the rehabilitation program (Figure 3).


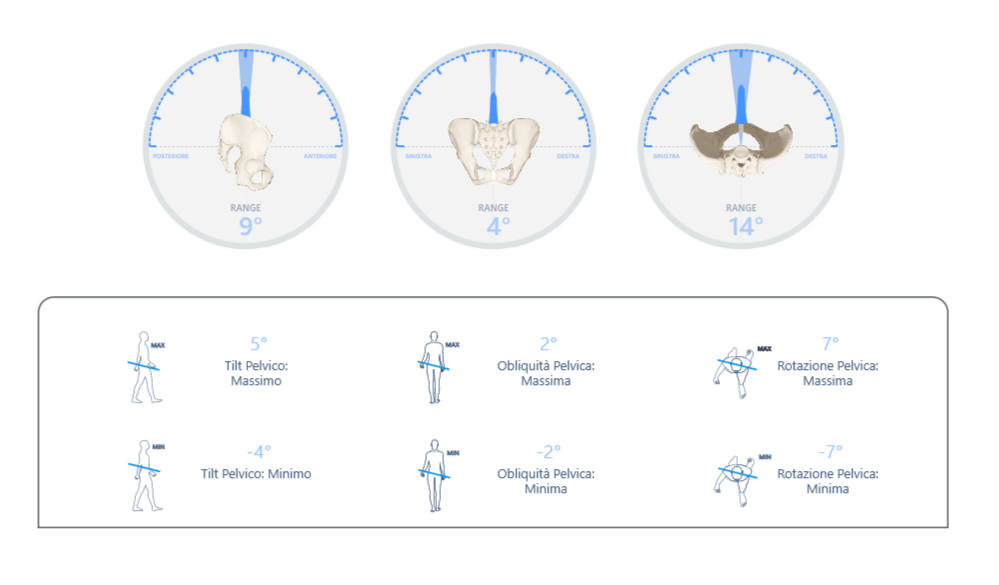
Figure 3: gait analysis with baiobit
The examination performed shows:
- decreased walking speed,0.56 m / s, below the normal values, highlighting a high degree of instability;
- decreased propulsion, 2.72 and 1.64, for the left and right respectively, both below the normal value;
- stride length normalized to height was below normal values (66% bilaterally), possibly linked to the very short flight phase due to an excessive search for stability;
- imbalances during the gait cycle phases, with an increase in the support phase, in particular the double support phases, supporting the hypothesis of an excessive search for stability.
Therefore, the next rehabilitation process will be aimed at improving the strength in the lower limbs to allow an adequate propulsion, and training in the management of dynamic balance, in order to allow proper length and stride phase management.
BIBLIOGRAPHY
1. Ibrahim, M. S., Alazzawi, S., Nizam, I., & Haddad, F. S. (2013). An evidence-based review of enhanced recovery interventions in knee replacement surgery. The Annals of The Royal College of Surgeons of England, 95(6), 386-389.
2. Castrodad, I. M. D., Recai, T. M., Abraham, M. M., Etcheson, J. I., Mohamed, N. S., Edalatpour, A., & Delanois, R. E. (2019). Rehabilitation protocols following total knee arthroplasty: a review of study designs and outcome measures. Annals of translational medicine, 7(Suppl 7).
3. Ebert, J. R., Munsie, C., & Joss, B. (2014). Guidelines for the early restoration of active knee flexion after total knee arthroplasty: implications for rehabilitation and early intervention. Archives of physical medicine and rehabilitation, 95(6), 1135-1140.
4. Barker, K. L., Hannink, E., Pemberton, S., & Jenkins, C. (2018). Knee arthroplasty patients predicted versus actual recovery: what are their expectations about time of recovery after surgery and how long before they can do the tasks they want to do?. Archives of physical medicine and rehabilitation, 99(11), 2230-2237.
5. Wainwright, T. W., Gill, M., McDonald, D. A., Middleton, R. G., Reed, M., Sahota, O., ... & Ljungqvist, O. (2020). Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Acta orthopaedica, 91(1), 3-19.
6. Valtonen, A., Pöyhönen, T., Sipilä, S., & Heinonen, A. (2010). Effects of aquatic resistance training on mobility limitation and lower-limb impairments after knee replacement. Archives of physical medicine and rehabilitation, 91(6), 833-839.